Alcoholism is one of the most misunderstood conditions in modern society. Historically, many believed that excessive drinking was simply a sign of poor self-control or a lack of discipline. However, decades of scientific research have proven otherwise. Alcohol use disorder (AUD) is a chronic disease that alters brain function, leading to compulsive alcohol consumption despite adverse consequences. This concept is the foundation of the disease theory of alcoholism, which recognizes addiction as a medical condition rather than a personal weakness.1
This theory has had a profound impact on how healthcare professionals diagnose, treat, and support individuals struggling with alcohol addiction. By understanding alcoholism as a disease, treatment approaches have shifted from punitive measures to evidence-based medical and psychological interventions that address both the physical and behavioral aspects of addiction.2
At Pathways Recovery Center, we provide comprehensive, science-backed treatment for individuals seeking to regain control of their lives. Recognizing alcoholism as a disease helps individuals and their families move away from shame and stigma and toward effective recovery solutions that promote long-term healing.
Understanding the Disease Theory of Alcoholism
The disease theory of alcoholism proposes that alcohol addiction is not simply a result of poor decision-making or a lack of willpower but rather a chronic medical condition with identifiable biological and psychological causes. This theory acknowledges that specific individuals have a higher susceptibility to alcohol dependence due to genetic predisposition, brain chemistry, and environmental influences. Instead of viewing excessive drinking as a personal failing, the disease model emphasizes that alcoholism follows a predictable progression, often beginning with occasional or social drinking before escalating into dependency.
For some, this progression can lead to becoming a functioning alcoholic, where an individual continues to manage daily responsibilities—such as work, family, and social obligations—while struggling with alcohol dependence. Despite maintaining an outward appearance of control, functioning alcoholics often experience increased cravings, higher tolerance, and difficulty moderating their drinking. Without intervention, alcoholism can worsen over time, reinforcing the importance of comprehensive treatment to achieve long-term recovery.
Leading medical organizations, including the American Medical Association (AMA) and the National Institute on Alcohol Abuse and Alcoholism (NIAAA), classify alcoholism as a disease based on specific criteria: 3,4
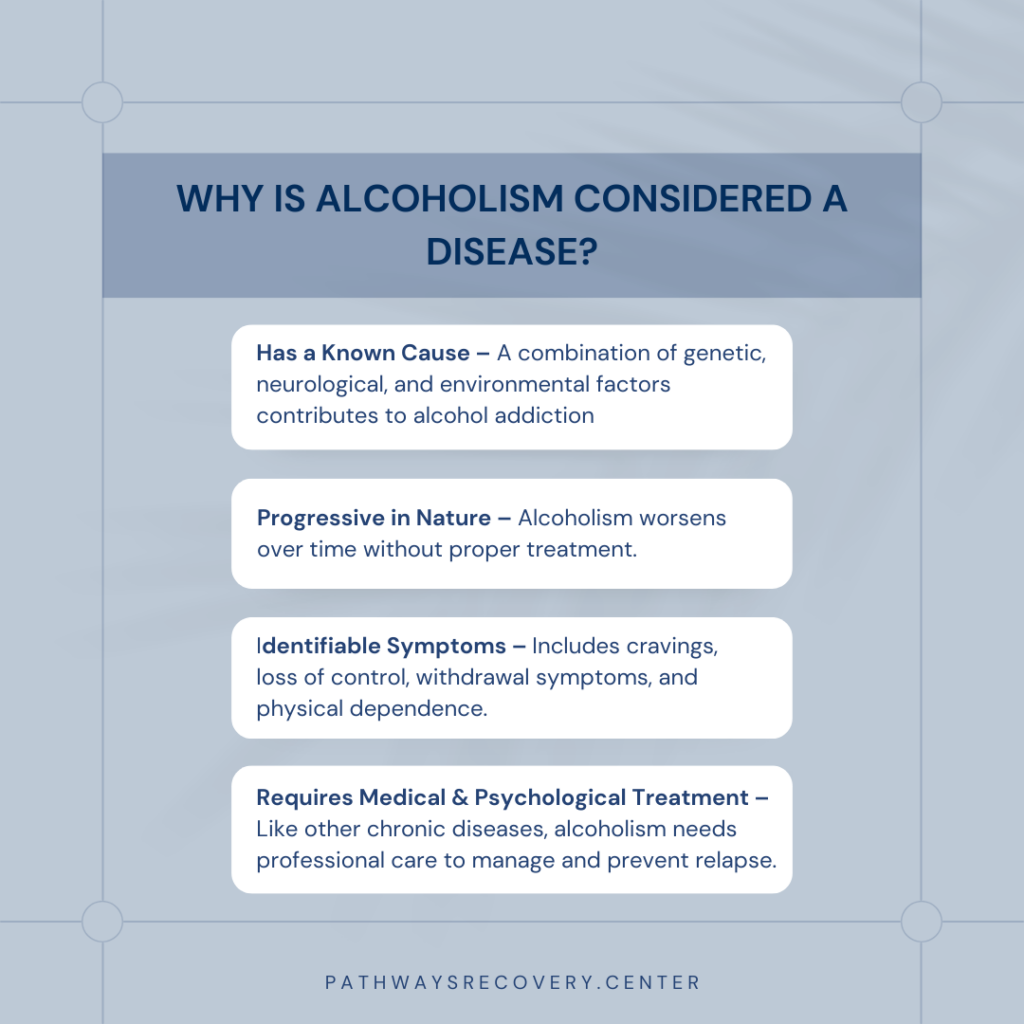
- A Known Cause – Alcoholism develops due to a combination of genetic, neurological, and environmental risk factors. Family history, mental health conditions, and repeated alcohol exposure all contribute to the likelihood of developing alcohol use disorder.
- A Progressive Course – Without intervention, alcoholism worsens over time, leading to increasing physical dependence, escalating alcohol consumption, and severe health complications.
- Identifiable Symptoms – Alcoholism presents with apparent symptoms, including uncontrollable cravings, withdrawal symptoms when not drinking, and an inability to moderate alcohol use despite negative consequences.
Like other chronic diseases such as diabetes, hypertension, or heart disease, alcoholism requires ongoing treatment and management to prevent relapse and sustain long-term health. The disease theory of alcoholism underscores the need for structured medical intervention, behavioral therapy, and lifestyle adjustments to support individuals in maintaining sobriety.
The Science Behind Alcoholism as a Disease
Scientific research has confirmed that alcoholism is not just a behavioral issue—it is a complex disease that alters brain function, disrupts neurological pathways, and is influenced by both genetic and environmental factors.5 Alcohol use disorder (AUD) develops over time as alcohol consumption fundamentally changes the brain’s chemistry, making it increasingly difficult for individuals to control their drinking. Understanding these biological and environmental influences is essential for developing effective treatments that address the root causes of addiction rather than simply treating the symptoms.
How Alcohol Affects the Brain
Chronic alcohol consumption rewires critical areas of the brain, reinforcing compulsive drinking behaviors and making it extremely difficult to stop, even when an individual is aware of the negative consequences. Several key regions of the brain are affected by prolonged alcohol use:
- The Prefrontal Cortex – This part of the brain is responsible for decision-making, impulse control, and rational thought. Alcohol weakens its function, leading to impaired judgment, increased risk-taking, and reduced ability to resist cravings.6 As alcohol dependency develops, individuals find it harder to regulate their drinking behavior.
- The Limbic System – This area regulates emotions, motivation, and pleasure-seeking behaviors. Alcohol hijacks the brain’s natural reward system, flooding it with dopamine and reinforcing drinking as a pleasurable activity. Over time, the brain becomes reliant on alcohol to trigger feelings of reward and satisfaction, contributing to compulsive drinking.
- The Brain’s Neurotransmitters – Alcohol disrupts the balance of key brain chemicals, particularly dopamine, GABA (gamma-aminobutyric acid), and glutamate.7 These neurotransmitters regulate mood, relaxation, and anxiety levels, and alcohol temporarily enhances their effects. However, prolonged alcohol use depletes natural neurotransmitter production, leading to withdrawal symptoms, increased anxiety, and a higher risk of relapse when drinking stops.
Because these changes are physical and long-lasting, overcoming alcoholism is not just about willpower. The brain adapts to alcohol dependence, requiring medical detox, behavioral therapy, and long-term treatment strategies to support recovery and prevent relapse.
Genetic and Environmental Risk Factors
Alcoholism develops through a combination of genetic susceptibility and environmental influences, making some individuals more vulnerable than others. Research suggests that genetics account for 40-60% of a person’s risk of developing alcohol use disorder, meaning that those with a family history of alcoholism are at a significantly higher risk.8 However, genetics alone do not determine whether a person will become addicted—environmental factors also play a crucial role in shaping drinking behaviors.
Some of the most significant environmental risk factors include:
- Early Exposure to Alcohol – Individuals who begin drinking at a young age are more likely to develop problematic drinking patterns later in life. Early alcohol use primes the brain for dependency, increasing the likelihood of addiction.
- High-Stress Environments and Trauma – Chronic stress, unresolved trauma, or exposure to abuse can lead individuals to use alcohol as a coping mechanism. Over time, this behavior can evolve into dependency, as the brain associates alcohol with emotional relief.
- Peer Pressure and Social Drinking Culture – The influence of friends, coworkers, or cultural norms can encourage heavy drinking, particularly in environments where alcohol consumption is normalized. Social drinking can escalate into addiction, especially for those already predisposed to alcoholism.
- Co-Occurring Mental Health Disorders – Many individuals struggling with alcoholism also experience conditions such as depression, anxiety, PTSD, or bipolar disorder. Alcohol is often used as a form of self-medication, providing temporary relief from emotional distress. However, it ultimately worsens mental health symptoms and reinforces the cycle of addiction.
Since both genetic and environmental factors play a role in the development of alcoholism, treatment must take a holistic approach, addressing not just drinking behaviors but also underlying psychological, biological, and social factors. Without proper intervention, chronic alcohol abuse can progress to end-stage alcoholism, where severe physical and mental deterioration makes recovery more challenging. Effective recovery programs focus on identifying personal risk factors, developing coping mechanisms, and providing medical support to restore brain function and promote long-term sobriety.
Why the Disease Model of Alcoholism Matters
Reducing Stigma and Guilt
One of the most significant benefits of understanding alcoholism as a disease is the reduction of shame and stigma associated with addiction. Many individuals struggling with alcohol use disorder blame themselves, believing their drinking is a result of weak willpower or a personal failing. This misunderstanding often prevents people from seeking the help they need, as they may feel judged or unworthy of support. However, when alcoholism is recognized as a medical condition rather than a moral flaw, individuals are more likely to seek treatment without fear of condemnation.
Shifting societal attitudes toward addiction fosters a more compassionate, science-based perspective. When families, friends, and communities understand that alcoholism has biological, neurological, and psychological components, conversations around recovery become more supportive and less punitive. Recognizing that alcohol addiction is a disease allows individuals to access the medical and therapeutic interventions necessary for lasting recovery rather than feeling trapped by guilt and isolation.
Improving Treatment Approaches
Viewing alcoholism as a disease also transforms how treatment is approached. Instead of expecting individuals to stop drinking on their own, effective treatment simply acknowledges the biological and psychological complexities of addiction and provides structured, evidence-based care. Medical detox programs help manage withdrawal symptoms safely under supervision, reducing the risks associated with sudden alcohol cessation. Therapy and counseling are essential components of treatment as they address the underlying causes of addiction, such as trauma, mental health conditions, and learned behaviors.
Medication-assisted treatment (MAT) can also play a vital role in recovery by reducing alcohol cravings and lowering the risk of relapse. For many individuals, long-term sobriety is supported by peer-based recovery programs, where participation in support groups provides encouragement, accountability, and shared experiences that reinforce the commitment to sobriety.
At Pathways Recovery Center, we take a holistic approach to alcohol addiction treatment, combining medical care, therapy, and peer support to help individuals achieve lasting recovery. Understanding alcoholism as a disease allows for treatment plans that are tailored to each person’s unique needs, ensuring a comprehensive path to healing rather than a one-size-fits-all solution.
Common Misconceptions About the Disease Model
Despite overwhelming scientific evidence, misconceptions about alcoholism persist, leading to harmful stigma and misunderstandings about addiction. Many people continue to view alcohol dependence as a personal failing rather than a medical condition, which can discourage those struggling with alcohol use disorder from seeking help. By addressing these myths, we can foster a better understanding of the disease theory of alcoholism and promote more effective approaches to recovery.
Myth #1: “Alcoholism Is Just a Choice”
A common belief is that alcoholism is a conscious decision and that individuals struggling with alcohol addiction can stop drinking whenever they choose. While the initial decision to drink may be voluntary, addiction develops as alcohol rewires brain function, creating physical and psychological dependence. As alcohol use progresses, the brain’s reward system becomes conditioned to crave and seek alcohol compulsively, making it increasingly difficult to stop drinking without professional intervention. Over time, drinking becomes less about choice and more about the body’s biological need for alcohol to function normally.
Myth #2: “People With Willpower Can Stop Drinking Anytime”
Alcoholism is often misunderstood as a lack of discipline or self-control. However, scientific research has shown that addiction alters brain chemistry, impairing an individual’s ability to stop drinking, even when they want to.9 Chronic alcohol use affects the prefrontal cortex, which governs decision-making and impulse control, making it harder for individuals to resist cravings. Withdrawal symptoms—such as anxiety, nausea, tremors, and even seizures—can make quitting alcohol dangerous without medical supervision. Successful recovery requires a combination of medical detox, behavioral therapy, and ongoing support—not just willpower.
Myth #3: “Only Weak People Become Alcoholics”
Alcohol addiction does not discriminate—it can affect people from all backgrounds, including professionals, athletes, and high-achieving individuals. Genetics, mental health conditions, and environmental influences all contribute to a person’s risk of developing alcohol use disorder. 10 Many individuals struggling with alcoholism have underlying mental health conditions such as anxiety, depression, or PTSD, which increase susceptibility to substance use as a coping mechanism. Others may have a family history of alcoholism, leading them to believe that alcoholism is hereditary. While genetics can play a role in increasing vulnerability, environmental factors and personal experiences also shape a person’s relationship with alcohol. Recognizing that alcoholism is a medical disorder, not a sign of weakness, allows for more effective, science-based treatment approaches that support long-term recovery.
The Role of Professional Treatment in Recovery
Because alcoholism is a disease, it requires comprehensive, evidence-based treatment to effectively manage withdrawal symptoms, address underlying causes, and support long-term sobriety. Many individuals struggling with alcohol addiction attempt to quit on their own but find themselves trapped in a cycle of relapse and withdrawal. Without proper treatment, alcohol dependence can lead to severe health complications, emotional distress, and a diminished quality of life. Professional treatment provides the medical, psychological, and emotional support to break this cycle and promote sustainable recovery.
At Pathways Recovery Center, we offer a continuum of care designed to meet individuals at every stage of recovery. Our treatment programs include:
Medication-Assisted Detox
Withdrawal from alcohol can be dangerous and, in severe cases, even life-threatening. Medication-assisted detox (MAT) helps manage symptoms such as tremors, seizures, nausea, and anxiety, allowing individuals to transition into sobriety safely under medical supervision. Detox is the first critical step in recovery, ensuring that individuals can begin treatment with a stable foundation.
Inpatient Rehabilitation
For individuals who need structured, immersive treatment, inpatient rehabilitation provides 24/7 medical and therapeutic support in a controlled environment. This setting allows individuals to focus on healing without distractions or triggers that may contribute to relapse. Inpatient programs address both the physical and psychological aspects of addiction, ensuring that recovery is comprehensive and sustainable.
Individual and Group Therapy
Therapy is a cornerstone of alcohol addiction treatment, helping individuals uncover the root causes of their addiction and develop effective coping strategies. Cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and trauma-informed approaches are commonly used to help individuals manage cravings, address emotional triggers, and build resilience. Group therapy fosters community and peer support, allowing individuals to connect with others who share similar experiences.
Family Support Programs
Alcoholism affects more than just the individual—it impacts families, relationships, and loved ones. Family therapy and educational programs help rebuild trust, improve communication, and provide loved ones with the tools to support long-term recovery. Understanding the disease theory of alcoholism can empower family members to approach addiction with compassion and knowledge rather than frustration or blame.
By recognizing that alcoholism is a disease, individuals can take the first step toward recovery without shame or guilt. With personalized treatment, ongoing support, and a commitment to healing, lasting sobriety is not only possible—it is achievable. At Pathways Recovery Center, we provide the tools and guidance needed for individuals to reclaim their lives and build a future free from alcohol dependence.
Alcohol Addiction Treatment at Pathways Recovery Center
At Pathways Recovery Center in Los Angeles County, we recognize alcoholism as a disease that requires comprehensive, individualized treatment. Our approach goes beyond simply addressing alcohol use—we focus on the physical, emotional, and psychological factors that contribute to addiction. Combining medical detox, evidence-based therapy, and holistic support, we help individuals achieve lasting recovery and regain control of their lives.
Our team of medical professionals, therapists, and addiction specialists is dedicated to providing compassionate, science-backed care tailored to each individual’s unique needs. Whether you require medication-assisted detox, inpatient rehabilitation, or long-term recovery planning, we are here to support you at every stage of your journey.
If you or a loved one is struggling with alcohol addiction, know that you don’t have to face it alone. Understanding the disease theory of alcoholism allows individuals to seek treatment without shame or stigma, knowing that recovery is possible with the proper support.
Take the first step today. Contact Pathways Recovery Center to learn more about our alcohol addiction treatment programs and begin your path to a healthier, alcohol-free future.
References:
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8357831/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC2916744/
- https://www.ama-assn.org/
- https://www.niaaa.nih.gov/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4040959/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3593065/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6826822/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC2442454/
- https://www.niaaa.nih.gov/health-professionals-communities/core-resource-on-alcohol/neuroscience-brain-addiction-and-recovery
- https://www.niaaa.nih.gov/health-professionals-communities/core-resource-on-alcohol/risk-factors-varied-vulnerability-alcohol-related-harm